Women most at risk
More than 90 percent of people with lupus are
women between the ages of 15 and 44. It’s more
common among women of African American,
Hispanic, Asian and Native American descent than
among Caucasian women.
Doctors don’t yet know what causes lupus.
Research points to a combination of inherited
characteristics and environmental factors. Viruses,
allergies, stress, medicines and even sunlight
seem to play some role.
6
W I N T E R 2 0 1 5
T H E
S A M A R I T A N
Keeping flares at bay
Lupus symptoms typically
come and go. When things
are relatively quiet, it’s
called remission. When
symptoms surge, it’s called
a flare.
Flares aren’t always
predictable.
Still, if you learn what’s
likely to cause a flare, you
can often take steps to
limit its severity. Common
triggers include:
■
Working too much.
■
Not getting enough
rest.
■
Feeling stressed.
■
Staying out in the sun too
long.
■
Taking certain types of
medications.
■
Getting an infection.
Predicting flares
Some people notice certain
signs of an impending
flare. These may include
body aches, stomachache,
headache, fever, unex-
plained rash or unusual
amounts of fatigue. It’s
important to call your doc-
tor right away if you feel a
flare coming on.
The best way to prevent
lupus flares is to follow your
treatment plan. That will
likely include:
■
Having regular doctor
visits.
■
Getting plenty of rest.
■
Eating a healthy diet.
■
Exercising, as your doctor
recommends.
■
Taking medication.
Seek support
But even people who
closely follow their
treatment plan can
sometimes get flares.
That unpredictability can
lead to anger, sadness
and depression.
That’s one of the rea-
sons it’s important to reach
out for support from people
you trust, including family
and friends.
Taking part in a struc-
tured support group or
getting one-on-one counsel-
ing from a mental health
professional can also help
you cope.
Sources: American Academy of Family
Physicians; American College of
Rheumatology; National Institutes
of Health
IS IT LUPUS?
Signs and symptoms o en
mimic other diseases
THE BODY HAS
an amazing ability to fight off germs
and other harmful agents. But sometimes, for reasons
not fully understood, the immune system instead tar-
gets healthy tissues, leading to pain, inflammation and
organ damage.
When a person’s immune system misfires in this way,
he or she is said to have an autoimmune disease. One of
the more challenging diseases of this type is lupus—a
chronic, complex, often life-altering condition that can
cause a wide range of symptoms.
So far, there is no cure. But almost everyone with lu-
pus can be treated to improve his or her quality of life.
SOLVING THE MYSTERY
Lupus can affect many parts
of the body. Often, joints, kidneys and skin are the main
targets. Most people with lupus report severe fatigue,
arthritis, fever and rashes.
The list of possible lupus signs and symptoms includes:
●
Anemia.
●
Kidney problems.
●
Chest pain.
●
Sensi-
tivity to sunlight.
●
Hair loss.
●
Eye problems.
●
Poor
circulation in fingers and toes.
●
Swelling in the legs or
around the eyes.
●
Mouth sores.
Lupus often comes on slowly. Signs and symptoms can
come and go and may change over time.
A lupus diagnosis can be difficult, in part because so
many of the signs and symptoms are similar to those of
other ailments. And there is no single, definitive test for
the disease. When doctors suspect lupus, they’re likely to:
●
Order a series of blood tests and other lab work, which
may include tissue biopsies.
●
Examine a patient’s medical history.
●
Do a complete physical exam.
INDIVIDUALIZED TREATMENT
People with lupus receive
treatment according to their symptoms. For example,
some may need medicine for inflammation, pain and
fever. Others may need more aggressive treatments to
thwart damage to the heart, kidneys or other organs.
In addition to a primary care doctor, lupus patients
often see other medical specialists, including experts in
joint pain, skin ailments and immune system disorders.
Beyond medicine, treatment may also include lifestyle
changes that help people better cope with the disease.
Changes in diet, exercise and stress management can all
help people live well with lupus.
Sources: American Academy of Family Physicians; American College of Rheumatology; National
Institutes of Health
VASCULITIS
WHAT’S THAT?
is rare condition can have
some serious consequences
IT’S GREAT WHEN
your heart is set aflame by love.
It’s not so good if your blood vessels become inflamed
because of disease.
In some cases this inflammation stems from a condi-
tion called vasculitis.
There are more than 20 types of vasculitis. Each type
affects vessels in different parts of the body. All types of
vasculitis are set off when the immune system accidentally
attacks the blood vessels.
No one is sure what sets this process in motion. What
is known is that once your blood vessels are inflamed,
you can have pain, redness, swelling and a host of other
symptoms. And you may lose some function in the af-
fected area.
Vasculitis also places you at higher risk for an aneu-
rysm (a bulge in the wall of a blood vessel) and poor or
even blocked blood flow. If left untreated, most forms of
vasculitis are deadly.
Here are some other brief basics to help you better
understand this condition.
WHO’S AT RISK?
Even though there are many kinds of
vasculitis, overall the condition is rare.
You’re most at risk for it if you:
●
Have certain chronic diseases, such as hepatitis B or C.
●
Have an autoimmune disorder, like lupus, rheumatoid
arthritis or scleroderma.
●
Are a smoker.
Each type of vasculitis has unique symptoms. How-
ever, in general most types of vasculitis cause:
●
Fever.
●
Loss of appetite.
●
Weight loss.
●
Tiredness.
●
General aches and pains.
HOW IS IT DIAGNOSED AND TREATED?
Many tests are
used to diagnose vasculitis. You might have blood tests,
a biopsy or imaging tests.
And because vasculitis is complex and not
common, you may need to see a specialist to get properly
diagnosed.
Some people will only need over-the-counter anti-
inflammatory medications, such as ibuprofen, to combat
vasculitis. Others will be prescribed corticosteroids or
cytotoxic medicines (which kill the cells that are causing
the inflammation).
Some patients will recover with treatment. Others
will find that the condition goes into an inactive state
(remission).
Research is adding to the treatment options for this
condition. And doctors are working to better understand
the process behind vasculitis.
Learn more by visiting the website of the American
College of Rheumatology at
www.rheumatology.org.
Click on “Patient Resources.”
Additional source: National Institutes of Health
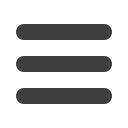
Where lupus can strike the body
Do you have these symptoms?
If you need to nd a doctor, call Samaritan
Family Medicine at
-
or go to
www.samaritanhealthcare.com/physicians.Brain
Skin
Heart
Lungs
Kidneys
Blood
vessels
Joints
Coffey
infographic
with
information
from the
National
Institutes of
Health

















